Shared on 29-02-2020
All about Liver Chirrhosis
All about Liver Chirrhosis
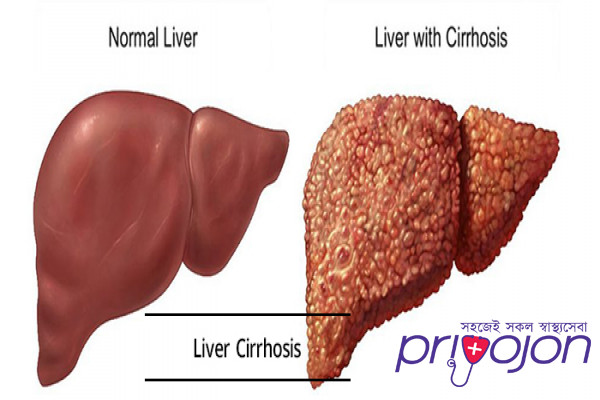
Cirrhosis, also known as liver cirrhosis or hepatic cirrhosis, is a condition in which the liver does not function properly due to long-term damage.[1] This damage is characterized by the replacement of normal liver tissue by scar tissue.[1] Typically, the disease develops slowly over months or years.[1] Early on, there are often no symptoms.[1] As the disease worsens, a person may become tired, weak, itchy, have swelling in the lower legs, develop yellow skin, bruise easily, have fluid build up in the abdomen, or develop spider-like blood vessels on the skin.[1] The fluid build-up in the abdomen may become spontaneously infected.[1] Other serious complications include hepatic encephalopathy, bleeding from dilated veins in the esophagus or dilated stomach veins, and liver cancer.[1] Hepatic encephalopathy results in confusion and may lead to unconsciousness.[1]
Cirrhosis is most commonly caused by alcohol, hepatitis B, hepatitis C, and non-alcoholic fatty liver disease.[1][2] Typically, more than two or three alcoholic drinks per day over a number of years is required for alcoholic cirrhosis to occur.[1] Non-alcoholic fatty liver disease has a number of causes, including being overweight, diabetes, high blood fats, and high blood pressure.[1] A number of less common causes of cirrhosis include autoimmune hepatitis, primary biliary cholangitis, hemochromatosis, certain medications, and gallstones.[1] Diagnosis is based on blood testing, medical imaging, and liver biopsy.[1]
Some causes of cirrhosis, such as hepatitis B, can be prevented by vaccination.[1] Treatment partly depends on the underlying cause,[1] but the goal is often to prevent worsening and complications.[1] Avoiding alcohol is recommended in all cases of cirrhosis.[1] Hepatitis B and C may be treatable with antiviral medications.[1] Autoimmune hepatitis may be treated with steroid medications.[1] Ursodiol may be useful if the disease is due to blockage of the bile ducts.[1] Other medications may be useful for complications such as abdominal or leg swelling, hepatic encephalopathy, and dilated esophageal veins.[1] In severe cirrhosis, a liver transplant may be an option.[1]
Cirrhosis affected about 2.8 million people and resulted in 1.3 million deaths in 2015.[3][4] Of these deaths, alcohol caused 348,000, hepatitis C caused 326,000, and hepatitis B caused 371,000.[4] In the United States, more men die of cirrhosis than women.[1] The first known description of the condition is by Hippocrates in the 5th century BCE.[5] The term cirrhosis was invented in 1819, from a Greek word for the yellowish color of a diseased liver.[6]
Signs and symptoms
Cirrhosis has many possible manifestations. These signs and symptoms may be either a direct result of the failure of liver cells, or secondary to the resultant increased pressure in the blood vessels in the hepatic portal system (portal hypertension). Some manifestations of cirrhosis are nonspecific, and also occur in several unrelated conditions. Likewise, the absence of any signs does not rule out the possibility of cirrhosis.[7] Cirrhosis of the liver is slow and gradual in its development. It is usually well advanced before its symptoms are noticeable enough to cause alarm. Weakness and weight loss may be early symptoms.
Liver dysfunction
The following features are as a direct consequence of liver cells not functioning.
Spider angiomata or spider nevi are vascular lesions consisting of a central arteriole surrounded by many smaller vessels (hence the name "spider") and occur due to an increase in estradiol. One study found that spider angiomata occur in about 1/3 of cases.[8]
Palmar erythema is a reddening of palms at the thenar and hypothenar eminences also as a result of increased estrogen.[9]
Gynecomastia, or increase in breast gland size in men that is not cancerous, is caused by increased estradiol and can occur in up to 2/3 of patients.[10] This is different from increase in breast fat in overweight people.[11]
Hypogonadism, a decrease in male sex hormones may manifest as impotence, infertility, loss of sexual drive, and testicular atrophy, and can result from primary gonadal injury or suppression of hypothalamic/pituitary function. Hypogonadism is associated with cirrhosis due to alcoholism or hemochromatosis.[12]
Liver size can be enlarged, normal, or shrunken in people with cirrhosis.
Ascites, accumulation of fluid in the peritoneal cavity (space in the abdomen), gives rise to "flank dullness". This may be visible as an increase in abdominal girth.[13]
Fetor hepaticus is a musty breath odor resulting from increased dimethyl sulfide.[14]
Jaundice, or icterus is yellow discoloration of the skin and mucous membranes, (with the white of the eye being especially noticeable) due to increased bilirubin (at least 2–3 mg/dl or 30 µmol/l). The urine may also appear dark.[13]
Causes
Liver cirrhosis has many possible causes; sometimes more than one cause is present in the same person. Globally, 57% of cirrhosis is attributable to either hepatitis B (30%) or hepatitis C (27%).[19] Alcohol consumption is another major cause, accounting for about 20% of the cases.[19]
Alcoholic liver disease (ALD). Alcoholic cirrhosis develops for 10–20% of individuals who drink heavily for a decade or more.[20] Alcohol seems to injure the liver by blocking the normal metabolism of protein, fats, and carbohydrates. This injury happens through the formation of acetaldehyde from alcohol which itself is reactive, but which also leads to the accumulation of other reactive products in the liver.[13] Patients may also have concurrent alcoholic hepatitis with fever, hepatomegaly, jaundice, and anorexia. AST and ALT blood levels are both elevated, but at less than 300 IU/liter, with an AST:ALT ratio > 2.0, a value rarely seen in other liver diseases.[7] In the United States, 40% of cirrhosis-related deaths are due to alcohol.[13]
Non-alcoholic steatohepatitis (NASH). In NASH, fat builds up in the liver and eventually causes scar tissue. This type of hepatitis appears to be associated with obesity (40% of NASH patients) diabetes, protein malnutrition, coronary artery disease, and treatment with steroid medications. This disorder is similar in it signs to alcoholic liver disease, but the patient does not have an alcohol history. A biopsy is needed for diagnosis.[7]
Chronic hepatitis C. Infection with the hepatitis C virus causes inflammation of the liver and a variable grade of damage to the organ. Over several decades, this inflammation and damage can lead to cirrhosis. Among patients with chronic hepatitis C, 20–30% will develop cirrhosis.[13][21] Cirrhosis caused by hepatitis C and alcoholic liver disease are the most common reasons for liver transplant.[22]
Chronic hepatitis B. The hepatitis B virus causes liver inflammation and injury that over several decades can lead to cirrhosis. Hepatitis D is dependent on the presence of hepatitis B and accelerates cirrhosis in co-infection.[7]
Primary biliary cholangitis (also known as primary biliary cirrhosis). The bile ducts become damaged by an autoimmune process, leading to secondary liver damage. Patients may be asymptomatic or have fatigue, pruritus, and non-jaundice skin hyperpigmentation with hepatomegaly. There is prominent alkaline phosphatase elevation as well as elevations in cholesterol and bilirubin and usually positive anti-mitochondrial antibodies.
Primary sclerosing cholangitis. PSC is a progressive cholestatic disorder presenting with pruritus, steatorrhea, fat-soluble vitamin deficiencies, and metabolic bone disease. There is a strong association with inflammatory bowel disease (IBD), especially ulcerative colitis.[13]
Autoimmune hepatitis. This disease is caused by an attack of the liver by lymphocytes, causing inflammation and eventually scarring and cirrhosis. Findings include elevations in serum globulins, especially gamma globulins.[13]
Hereditary hemochromatosis. Usually presents with a family history of cirrhosis, skin hyperpigmentation, diabetes mellitus, pseudogout, or cardiomyopathy, all due to signs of iron overload.[13][23]
Wilson's disease. Autosomal recessive disorder characterized by low serum ceruloplasmin and increased hepatic copper content on liver biopsy and elevated 24-hour urine copper. May also have Kayser-Fleischer rings in the cornea and altered mental status.
Indian childhood cirrhosis is a form of neonatal cholestasis characterized by deposition of copper in the liver.[24]
Alpha 1-antitrypsin deficiency (A1AD). Autosomal recessive disorder of decreased levels of the enzyme alpha 1—antitrypsin.[13]
Cardiac cirrhosis. Due to chronic right sided heart failure, which leads to liver congestion.[13]
Galactosemia
Glycogen storage disease type IV
Cystic fibrosis[13]
Hepatotoxic drugs or toxins
Unestablished cause
There are some changes seen in cirrhosis whose causes are not clearly known. They may also be a sign of other non-liver related causes.
Nail changes.
Muehrcke's lines – paired horizontal bands separated by normal color resulting from hypoalbuminemia (inadequate production of albumin). It is not specific for cirrhosis.[15]
Terry's nails – proximal two-thirds of the nail plate appears white with distal one-third red, also due to hypoalbuminemia[16]
Clubbing – angle between the nail plate and proximal nail fold > 180 degrees. It is not specific for cirrhosis and can therefore be due to a number of conditions[16]
Hypertrophic osteoarthropathy. Chronic proliferative periostitis of the long bones that can cause considerable pain. It is not specific for cirrhosis.[16]
Dupuytren's contracture. Thickening and shortening of palmar fascia (tissue on the palm of the hands) that leads to flexion deformities of the fingers. Caused by fibroblastic proliferation (increased growth) and disorderly collagen deposition. It is relatively common (33% of patients).[16]
Other. Weakness, fatigue, loss of appetite, weight loss.[13]
Advanced disease
As the disease progresses, complications may develop. In some people, these may be the first signs of the disease.
Bruising and bleeding resulting from decreased production of coagulation factors.
Hepatic encephalopathy – occurs when ammonia and related substances build up in the blood and affect brain function when they are not cleared from the blood by the liver. This may result in neglect of personal appearance, unresponsiveness, forgetfulness, trouble concentrating, changes in sleep habits or psychosis. One classic physical exam findings is asterixis, bilateral asynchronous flapping of outstretched, dorsiflexed hands.[13]
Sensitivity to medication caused by decreased metabolism of the active compounds.
Acute kidney injury (particularly hepatorenal syndrome)[17]
Cachexia associated with muscle wasting and weakness[18]
Prevention
Key prevention strategies for cirrhosis are population-wide interventions to reduce alcohol intake (through pricing strategies, public health campaigns, and personal counseling), programs to reduce the transmission of viral hepatitis, and screening of relatives of people with hereditary liver diseases.[citation needed]
Little is known about factors affecting cirrhosis risk and progression. Research has suggested that coffee consumption appears to help protect against cirrhosis.[44][45]
Treatment
Generally, liver damage from cirrhosis cannot be reversed, but treatment can stop or delay further progression and reduce complications. A healthy diet is encouraged, as cirrhosis may be an energy-consuming process. Close follow-up is often necessary. Antibiotics are prescribed for infections, and various medications can help with itching. Laxatives, such as lactulose, decrease the risk of constipation; their role in preventing encephalopathy is limited.
Alcoholic cirrhosis caused by alcohol abuse is treated by abstaining from alcohol. Treatment for hepatitis-related cirrhosis involves medications used to treat the different types of hepatitis, such as interferon for viral hepatitis and corticosteroids for autoimmune hepatitis. Cirrhosis caused by Wilson's disease, in which copper builds up in organs, is treated with chelation therapy (for example, penicillamine) to remove the copper.
Preventing further liver damage
Regardless of the underlying cause of cirrhosis, consumption of alcohol and paracetamol (acetaminophen), as well as other potentially damaging substances, are discouraged. Vaccination of susceptible patients should be considered for Hepatitis A and Hepatitis B. Treating the cause of cirrhosis prevents further damage; for example, giving oral antivirals such as entecavir and tenofovir in patients of cirrhosis due to Hepatitis B prevents progression of cirrhosis. Similarly, control of weight and diabetes prevents deterioration in cirrhosis due to Non-alcoholic steatohepatitis.
Transplantation
If complications cannot be controlled or when the liver ceases functioning, liver transplantation is necessary. Survival from liver transplantation has been improving over the 1990s, and the five-year survival rate is now around 80%. The survival rate depends largely on the severity of disease and other medical risk factors in the recipient.[46] In the United States, the MELD score is used to prioritize patients for transplantation.[47] Transplantation necessitates the use of immune suppressants (ciclosporin or tacrolimus).
Decompensated cirrhosis
Manifestations of decompensation in cirrhosis include gastrointestinal bleeding, hepatic encephalopathy (HE), jaundice or ascites. In patients with previously stable cirrhosis, decompensation may occur due to various causes, such as constipation, infection (of any source), increased alcohol intake, medication, bleeding from esophageal varices or dehydration. It may take the form of any of the complications of cirrhosis listed below.
People with decompensated cirrhosis generally require admission to a hospital, with close monitoring of the fluid balance, mental status, and emphasis on adequate nutrition and medical treatment – often with diuretics, antibiotics, laxatives or enemas, thiamine and occasionally steroids, acetylcysteine and pentoxifylline.[48] Administration of saline is avoided, as it would add to the already high total body sodium content that typically occurs in cirrhosis. Life expectancy without liver transplant is low, at most 3 years.
Palliative care
Palliative care is specialized medical care that focuses on providing patients with relief from the symptoms, pain, and stress of a serious illness, such as cirrhosis. The goal of palliative care is to improve quality of life for both the patient and the patient's family and it is appropriate at any stage and for any type of cirrhosis.[49]
Especially in the later stages, people with cirrhosis experience significant symptoms such as abdominal swelling, itching, leg edema, and chronic abdominal pain which would be amenable for treatment through palliative care.[50] Because the disease is not curable without a transplant, palliative care can also help with discussions regarding the person's wishes concerning health care power of attorney, Do Not Resuscitate decisions and life support, and potentially hospice.[50] Despite proven benefit, people with cirrhosis are rarely referred to palliative care.[51]
Cirrhosis, also known as liver cirrhosis or hepatic cirrhosis, is a condition in which the liver does not function properly due to long-term damage.[1] This damage is characterized by the replacement of normal liver tissue by scar tissue.[1] Typically, the disease develops slowly over months or years.[1] Early on, there are often no symptoms.[1] As the disease worsens, a person may become tired, weak, itchy, have swelling in the lower legs, develop yellow skin, bruise easily, have fluid build up in the abdomen, or develop spider-like blood vessels on the skin.[1] The fluid build-up in the abdomen may become spontaneously infected.[1] Other serious complications include hepatic encephalopathy, bleeding from dilated veins in the esophagus or dilated stomach veins, and liver cancer.[1] Hepatic encephalopathy results in confusion and may lead to unconsciousness.[1]
Cirrhosis is most commonly caused by alcohol, hepatitis B, hepatitis C, and non-alcoholic fatty liver disease.[1][2] Typically, more than two or three alcoholic drinks per day over a number of years is required for alcoholic cirrhosis to occur.[1] Non-alcoholic fatty liver disease has a number of causes, including being overweight, diabetes, high blood fats, and high blood pressure.[1] A number of less common causes of cirrhosis include autoimmune hepatitis, primary biliary cholangitis, hemochromatosis, certain medications, and gallstones.[1] Diagnosis is based on blood testing, medical imaging, and liver biopsy.[1]
Some causes of cirrhosis, such as hepatitis B, can be prevented by vaccination.[1] Treatment partly depends on the underlying cause,[1] but the goal is often to prevent worsening and complications.[1] Avoiding alcohol is recommended in all cases of cirrhosis.[1] Hepatitis B and C may be treatable with antiviral medications.[1] Autoimmune hepatitis may be treated with steroid medications.[1] Ursodiol may be useful if the disease is due to blockage of the bile ducts.[1] Other medications may be useful for complications such as abdominal or leg swelling, hepatic encephalopathy, and dilated esophageal veins.[1] In severe cirrhosis, a liver transplant may be an option.[1]
Cirrhosis affected about 2.8 million people and resulted in 1.3 million deaths in 2015.[3][4] Of these deaths, alcohol caused 348,000, hepatitis C caused 326,000, and hepatitis B caused 371,000.[4] In the United States, more men die of cirrhosis than women.[1] The first known description of the condition is by Hippocrates in the 5th century BCE.[5] The term cirrhosis was invented in 1819, from a Greek word for the yellowish color of a diseased liver.[6]
Signs and symptoms
Cirrhosis has many possible manifestations. These signs and symptoms may be either a direct result of the failure of liver cells, or secondary to the resultant increased pressure in the blood vessels in the hepatic portal system (portal hypertension). Some manifestations of cirrhosis are nonspecific, and also occur in several unrelated conditions. Likewise, the absence of any signs does not rule out the possibility of cirrhosis.[7] Cirrhosis of the liver is slow and gradual in its development. It is usually well advanced before its symptoms are noticeable enough to cause alarm. Weakness and weight loss may be early symptoms.
Liver dysfunction
The following features are as a direct consequence of liver cells not functioning.
Spider angiomata or spider nevi are vascular lesions consisting of a central arteriole surrounded by many smaller vessels (hence the name "spider") and occur due to an increase in estradiol. One study found that spider angiomata occur in about 1/3 of cases.[8]
Palmar erythema is a reddening of palms at the thenar and hypothenar eminences also as a result of increased estrogen.[9]
Gynecomastia, or increase in breast gland size in men that is not cancerous, is caused by increased estradiol and can occur in up to 2/3 of patients.[10] This is different from increase in breast fat in overweight people.[11]
Hypogonadism, a decrease in male sex hormones may manifest as impotence, infertility, loss of sexual drive, and testicular atrophy, and can result from primary gonadal injury or suppression of hypothalamic/pituitary function. Hypogonadism is associated with cirrhosis due to alcoholism or hemochromatosis.[12]
Liver size can be enlarged, normal, or shrunken in people with cirrhosis.
Ascites, accumulation of fluid in the peritoneal cavity (space in the abdomen), gives rise to "flank dullness". This may be visible as an increase in abdominal girth.[13]
Fetor hepaticus is a musty breath odor resulting from increased dimethyl sulfide.[14]
Jaundice, or icterus is yellow discoloration of the skin and mucous membranes, (with the white of the eye being especially noticeable) due to increased bilirubin (at least 2–3 mg/dl or 30 µmol/l). The urine may also appear dark.[13]
Causes
Liver cirrhosis has many possible causes; sometimes more than one cause is present in the same person. Globally, 57% of cirrhosis is attributable to either hepatitis B (30%) or hepatitis C (27%).[19] Alcohol consumption is another major cause, accounting for about 20% of the cases.[19]
Alcoholic liver disease (ALD). Alcoholic cirrhosis develops for 10–20% of individuals who drink heavily for a decade or more.[20] Alcohol seems to injure the liver by blocking the normal metabolism of protein, fats, and carbohydrates. This injury happens through the formation of acetaldehyde from alcohol which itself is reactive, but which also leads to the accumulation of other reactive products in the liver.[13] Patients may also have concurrent alcoholic hepatitis with fever, hepatomegaly, jaundice, and anorexia. AST and ALT blood levels are both elevated, but at less than 300 IU/liter, with an AST:ALT ratio > 2.0, a value rarely seen in other liver diseases.[7] In the United States, 40% of cirrhosis-related deaths are due to alcohol.[13]
Non-alcoholic steatohepatitis (NASH). In NASH, fat builds up in the liver and eventually causes scar tissue. This type of hepatitis appears to be associated with obesity (40% of NASH patients) diabetes, protein malnutrition, coronary artery disease, and treatment with steroid medications. This disorder is similar in it signs to alcoholic liver disease, but the patient does not have an alcohol history. A biopsy is needed for diagnosis.[7]
Chronic hepatitis C. Infection with the hepatitis C virus causes inflammation of the liver and a variable grade of damage to the organ. Over several decades, this inflammation and damage can lead to cirrhosis. Among patients with chronic hepatitis C, 20–30% will develop cirrhosis.[13][21] Cirrhosis caused by hepatitis C and alcoholic liver disease are the most common reasons for liver transplant.[22]
Chronic hepatitis B. The hepatitis B virus causes liver inflammation and injury that over several decades can lead to cirrhosis. Hepatitis D is dependent on the presence of hepatitis B and accelerates cirrhosis in co-infection.[7]
Primary biliary cholangitis (also known as primary biliary cirrhosis). The bile ducts become damaged by an autoimmune process, leading to secondary liver damage. Patients may be asymptomatic or have fatigue, pruritus, and non-jaundice skin hyperpigmentation with hepatomegaly. There is prominent alkaline phosphatase elevation as well as elevations in cholesterol and bilirubin and usually positive anti-mitochondrial antibodies.
Primary sclerosing cholangitis. PSC is a progressive cholestatic disorder presenting with pruritus, steatorrhea, fat-soluble vitamin deficiencies, and metabolic bone disease. There is a strong association with inflammatory bowel disease (IBD), especially ulcerative colitis.[13]
Autoimmune hepatitis. This disease is caused by an attack of the liver by lymphocytes, causing inflammation and eventually scarring and cirrhosis. Findings include elevations in serum globulins, especially gamma globulins.[13]
Hereditary hemochromatosis. Usually presents with a family history of cirrhosis, skin hyperpigmentation, diabetes mellitus, pseudogout, or cardiomyopathy, all due to signs of iron overload.[13][23]
Wilson's disease. Autosomal recessive disorder characterized by low serum ceruloplasmin and increased hepatic copper content on liver biopsy and elevated 24-hour urine copper. May also have Kayser-Fleischer rings in the cornea and altered mental status.
Indian childhood cirrhosis is a form of neonatal cholestasis characterized by deposition of copper in the liver.[24]
Alpha 1-antitrypsin deficiency (A1AD). Autosomal recessive disorder of decreased levels of the enzyme alpha 1—antitrypsin.[13]
Cardiac cirrhosis. Due to chronic right sided heart failure, which leads to liver congestion.[13]
Galactosemia
Glycogen storage disease type IV
Cystic fibrosis[13]
Hepatotoxic drugs or toxins
Unestablished cause
There are some changes seen in cirrhosis whose causes are not clearly known. They may also be a sign of other non-liver related causes.
Nail changes.
Muehrcke's lines – paired horizontal bands separated by normal color resulting from hypoalbuminemia (inadequate production of albumin). It is not specific for cirrhosis.[15]
Terry's nails – proximal two-thirds of the nail plate appears white with distal one-third red, also due to hypoalbuminemia[16]
Clubbing – angle between the nail plate and proximal nail fold > 180 degrees. It is not specific for cirrhosis and can therefore be due to a number of conditions[16]
Hypertrophic osteoarthropathy. Chronic proliferative periostitis of the long bones that can cause considerable pain. It is not specific for cirrhosis.[16]
Dupuytren's contracture. Thickening and shortening of palmar fascia (tissue on the palm of the hands) that leads to flexion deformities of the fingers. Caused by fibroblastic proliferation (increased growth) and disorderly collagen deposition. It is relatively common (33% of patients).[16]
Other. Weakness, fatigue, loss of appetite, weight loss.[13]
Advanced disease
As the disease progresses, complications may develop. In some people, these may be the first signs of the disease.
Bruising and bleeding resulting from decreased production of coagulation factors.
Hepatic encephalopathy – occurs when ammonia and related substances build up in the blood and affect brain function when they are not cleared from the blood by the liver. This may result in neglect of personal appearance, unresponsiveness, forgetfulness, trouble concentrating, changes in sleep habits or psychosis. One classic physical exam findings is asterixis, bilateral asynchronous flapping of outstretched, dorsiflexed hands.[13]
Sensitivity to medication caused by decreased metabolism of the active compounds.
Acute kidney injury (particularly hepatorenal syndrome)[17]
Cachexia associated with muscle wasting and weakness[18]
Prevention
Key prevention strategies for cirrhosis are population-wide interventions to reduce alcohol intake (through pricing strategies, public health campaigns, and personal counseling), programs to reduce the transmission of viral hepatitis, and screening of relatives of people with hereditary liver diseases.[citation needed]
Little is known about factors affecting cirrhosis risk and progression. Research has suggested that coffee consumption appears to help protect against cirrhosis.[44][45]
Treatment
Generally, liver damage from cirrhosis cannot be reversed, but treatment can stop or delay further progression and reduce complications. A healthy diet is encouraged, as cirrhosis may be an energy-consuming process. Close follow-up is often necessary. Antibiotics are prescribed for infections, and various medications can help with itching. Laxatives, such as lactulose, decrease the risk of constipation; their role in preventing encephalopathy is limited.
Alcoholic cirrhosis caused by alcohol abuse is treated by abstaining from alcohol. Treatment for hepatitis-related cirrhosis involves medications used to treat the different types of hepatitis, such as interferon for viral hepatitis and corticosteroids for autoimmune hepatitis. Cirrhosis caused by Wilson's disease, in which copper builds up in organs, is treated with chelation therapy (for example, penicillamine) to remove the copper.
Preventing further liver damage
Regardless of the underlying cause of cirrhosis, consumption of alcohol and paracetamol (acetaminophen), as well as other potentially damaging substances, are discouraged. Vaccination of susceptible patients should be considered for Hepatitis A and Hepatitis B. Treating the cause of cirrhosis prevents further damage; for example, giving oral antivirals such as entecavir and tenofovir in patients of cirrhosis due to Hepatitis B prevents progression of cirrhosis. Similarly, control of weight and diabetes prevents deterioration in cirrhosis due to Non-alcoholic steatohepatitis.
Transplantation
If complications cannot be controlled or when the liver ceases functioning, liver transplantation is necessary. Survival from liver transplantation has been improving over the 1990s, and the five-year survival rate is now around 80%. The survival rate depends largely on the severity of disease and other medical risk factors in the recipient.[46] In the United States, the MELD score is used to prioritize patients for transplantation.[47] Transplantation necessitates the use of immune suppressants (ciclosporin or tacrolimus).
Decompensated cirrhosis
Manifestations of decompensation in cirrhosis include gastrointestinal bleeding, hepatic encephalopathy (HE), jaundice or ascites. In patients with previously stable cirrhosis, decompensation may occur due to various causes, such as constipation, infection (of any source), increased alcohol intake, medication, bleeding from esophageal varices or dehydration. It may take the form of any of the complications of cirrhosis listed below.
People with decompensated cirrhosis generally require admission to a hospital, with close monitoring of the fluid balance, mental status, and emphasis on adequate nutrition and medical treatment – often with diuretics, antibiotics, laxatives or enemas, thiamine and occasionally steroids, acetylcysteine and pentoxifylline.[48] Administration of saline is avoided, as it would add to the already high total body sodium content that typically occurs in cirrhosis. Life expectancy without liver transplant is low, at most 3 years.
Palliative care
Palliative care is specialized medical care that focuses on providing patients with relief from the symptoms, pain, and stress of a serious illness, such as cirrhosis. The goal of palliative care is to improve quality of life for both the patient and the patient's family and it is appropriate at any stage and for any type of cirrhosis.[49]
Especially in the later stages, people with cirrhosis experience significant symptoms such as abdominal swelling, itching, leg edema, and chronic abdominal pain which would be amenable for treatment through palliative care.[50] Because the disease is not curable without a transplant, palliative care can also help with discussions regarding the person's wishes concerning health care power of attorney, Do Not Resuscitate decisions and life support, and potentially hospice.[50] Despite proven benefit, people with cirrhosis are rarely referred to palliative care.[51]
Medically reviewed by
Dr. Rabeya Afroz Shomi
MBBS, FCPS, Dhaka Medical
3 Years of Experience
- Written by the Priyojon Editorial Team
